- Adrenal gland
- Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
-
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan Kwon Jung, Young Seok Cho, Jin Chul Paeng, Jae Hyeon Kim, Ohk-Hyun Ryu, Yumie Rhee, Chong Hwa Kim, Eun Jig Lee
-
Endocrinol Metab. 2021;36(2):322-338. Published online April 6, 2021
-
DOI: https://doi.org/10.3803/EnM.2020.908
-
-
7,504
View
-
572
Download
-
8
Web of Science
-
10
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
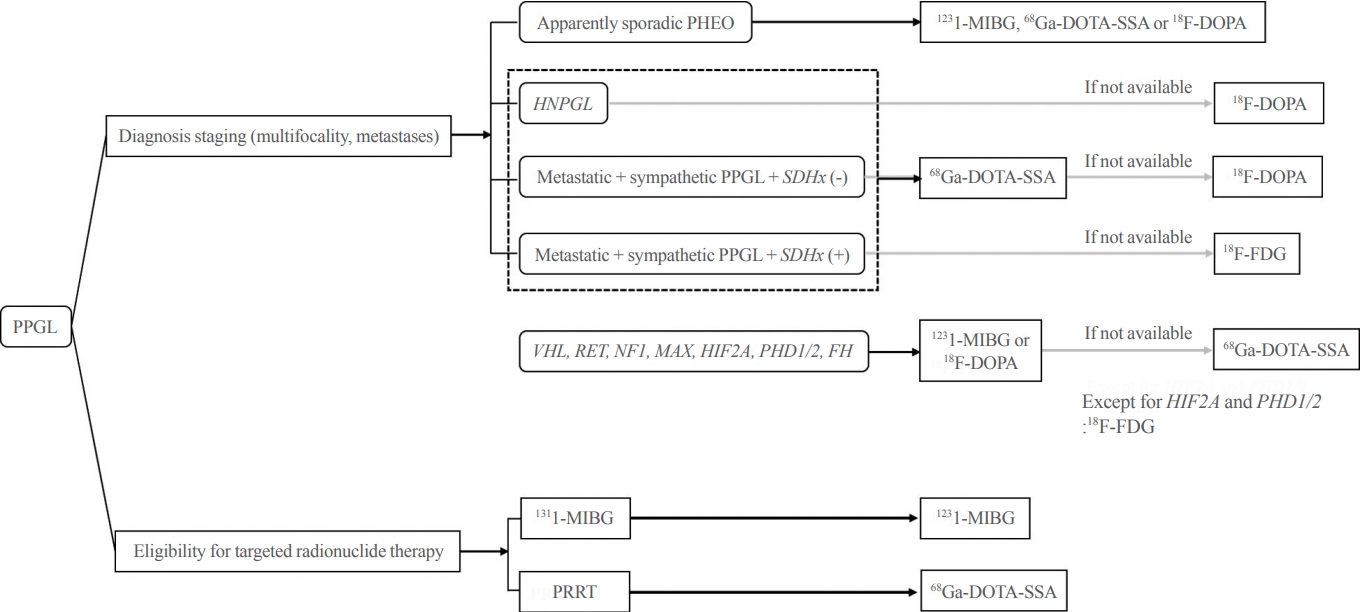
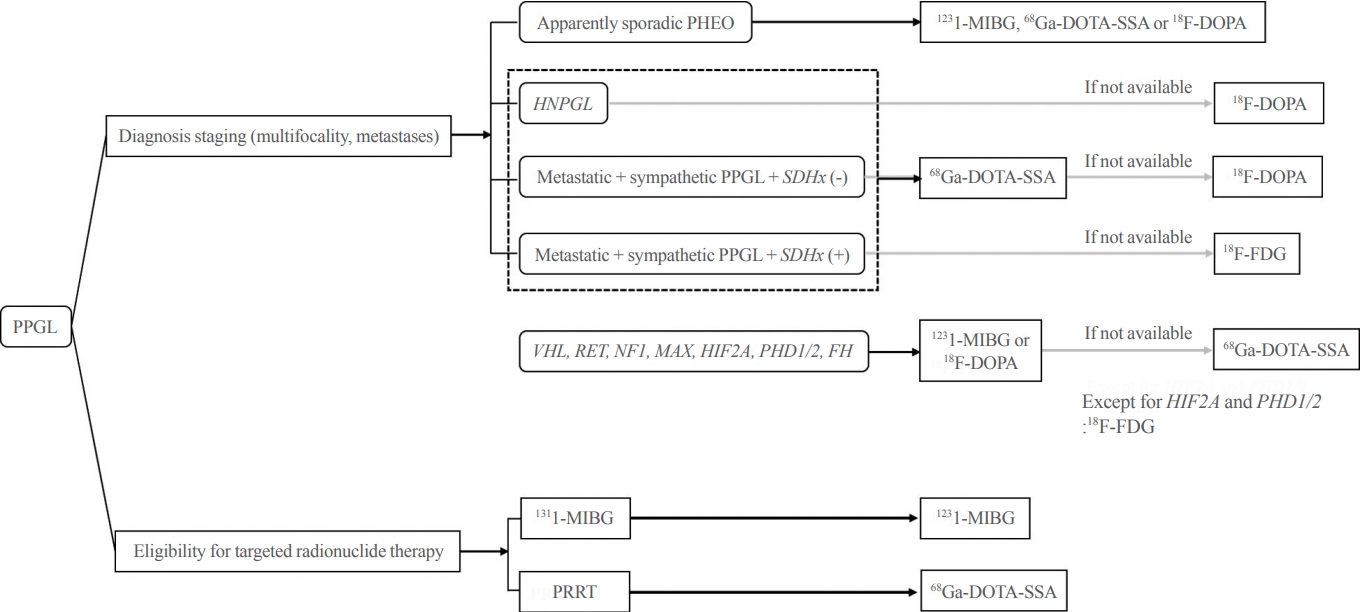
- Pheochromocytoma and paraganglioma (PPGLs) are rare catecholamine-secreting neuroendocrine tumors but can be life-threatening. Although most PPGLs are benign, approximately 10% have metastatic potential. Approximately 40% cases are reported as harboring germline mutations. Therefore, timely and accurate diagnosis of PPGLs is crucial. For more than 130 years, clinical, molecular, biochemical, radiological, and pathological investigations have been rapidly advanced in the field of PPGLs. However, performing diagnostic studies to localize lesions and detect metastatic potential can be still challenging and complicated. Furthermore, great progress on genetics has shifted the paradigm of genetic testing of PPGLs. The Korean PPGL task force team consisting of the Korean Endocrine Society, the Korean Surgical Society, the Korean Society of Nuclear Medicine, the Korean Society of Pathologists, and the Korean Society of Laboratory Medicine has developed this position statement focusing on the comprehensive and updated diagnosis for PPGLs.
-
Citations
Citations to this article as recorded by  - A Prospective Comparative Study of 18F-FDOPA PET/CT Versus 123I-MIBG Scintigraphy With SPECT/CT for the Diagnosis of Pheochromocytoma and Paraganglioma
Changhwan Sung, Hyo Sang Lee, Dong Yun Lee, Yong-il Kim, Jae Eun Kim, Sang Ju Lee, Seung Jun Oh, Tae-Yon Sung, Yu-Mi Lee, Young Hoon Kim, Beom-Jun Kim, Jung-Min Koh, Seung Hun Lee, Jin-Sook Ryu
Clinical Nuclear Medicine.2024; 49(1): 27. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
A Ram Hong, Ho-Cheol Kang
Endocrinology and Metabolism.2023; 38(2): 175. CrossRef - Lesion-based indicators predict long-term outcomes of pheochromocytoma and paraganglioma– SIZEPASS
Helena Hanschell, Salvador Diaz-Cano, Alfredo Blanes, Nadia Talat, Gabriele Galatá, Simon Aylwin, Klaus Martin Schulte
Frontiers in Endocrinology.2023;[Epub] CrossRef - Interleukin-6-producing paraganglioma as a rare cause of systemic inflammatory response syndrome: a case report
Yin Young Lee, Seung Min Chung
Journal of Yeungnam Medical Science.2023; 40(4): 435. CrossRef - (Extremely rare intrapericardial location of paraganglioma)
Jaroslav Zajíc, Aleš Mokráček, Ladislav Pešl, Jiří Haniš, Dita Schaffelhoferová
Cor et Vasa.2023; 65(4): 692. CrossRef - A Case of Von Hippel-Lindau Disease With Recurrence of Paraganglioma and No Other Associated Symptoms: The Importance of Genetic Testing and Establishing Follow-Up Policies
Naoki Okada, Akihiro Shioya, Sumihito Togi, Hiroki Ura, Yo Niida
Cureus.2023;[Epub] CrossRef - KSNM60 in Nuclear Endocrinology: from the Beginning to the Future
Chae Moon Hong, Young Jin Jeong, Hae Won Kim, Byeong-Cheol Ahn
Nuclear Medicine and Molecular Imaging.2022; 56(1): 17. CrossRef - Change of Computed Tomography-Based Body Composition after Adrenalectomy in Patients with Pheochromocytoma
Yousun Ko, Heeryoel Jeong, Seungwoo Khang, Jeongjin Lee, Kyung Won Kim, Beom-Jun Kim
Cancers.2022; 14(8): 1967. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Pheochromocytoma with Retroperitoneal Metastasis: A Case Report
建新 崔
Advances in Clinical Medicine.2021; 11(05): 2239. CrossRef
- Miscellaneous
- Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology
-
Jung Hee Kim, Hyun Wook Chae, Sang Ouk Chin, Cheol Ryong Ku, Kyeong Hye Park, Dong Jun Lim, Kwang Joon Kim, Jung Soo Lim, Gyuri Kim, Yun Mi Choi, Seong Hee Ahn, Min Ji Jeon, Yul Hwangbo, Ju Hee Lee, Bu Kyung Kim, Yong Jun Choi, Kyung Ae Lee, Seong-Su Moon, Hwa Young Ahn, Hoon Sung Choi, Sang Mo Hong, Dong Yeob Shin, Ji A Seo, Se Hwa Kim, Seungjoon Oh, Sung Hoon Yu, Byung Joon Kim, Choong Ho Shin, Sung-Woon Kim, Chong Hwa Kim, Eun Jig Lee
-
Endocrinol Metab. 2020;35(2):272-287. Published online June 24, 2020
-
DOI: https://doi.org/10.3803/EnM.2020.35.2.272
-
-
9,478
View
-
428
Download
-
13
Web of Science
-
15
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
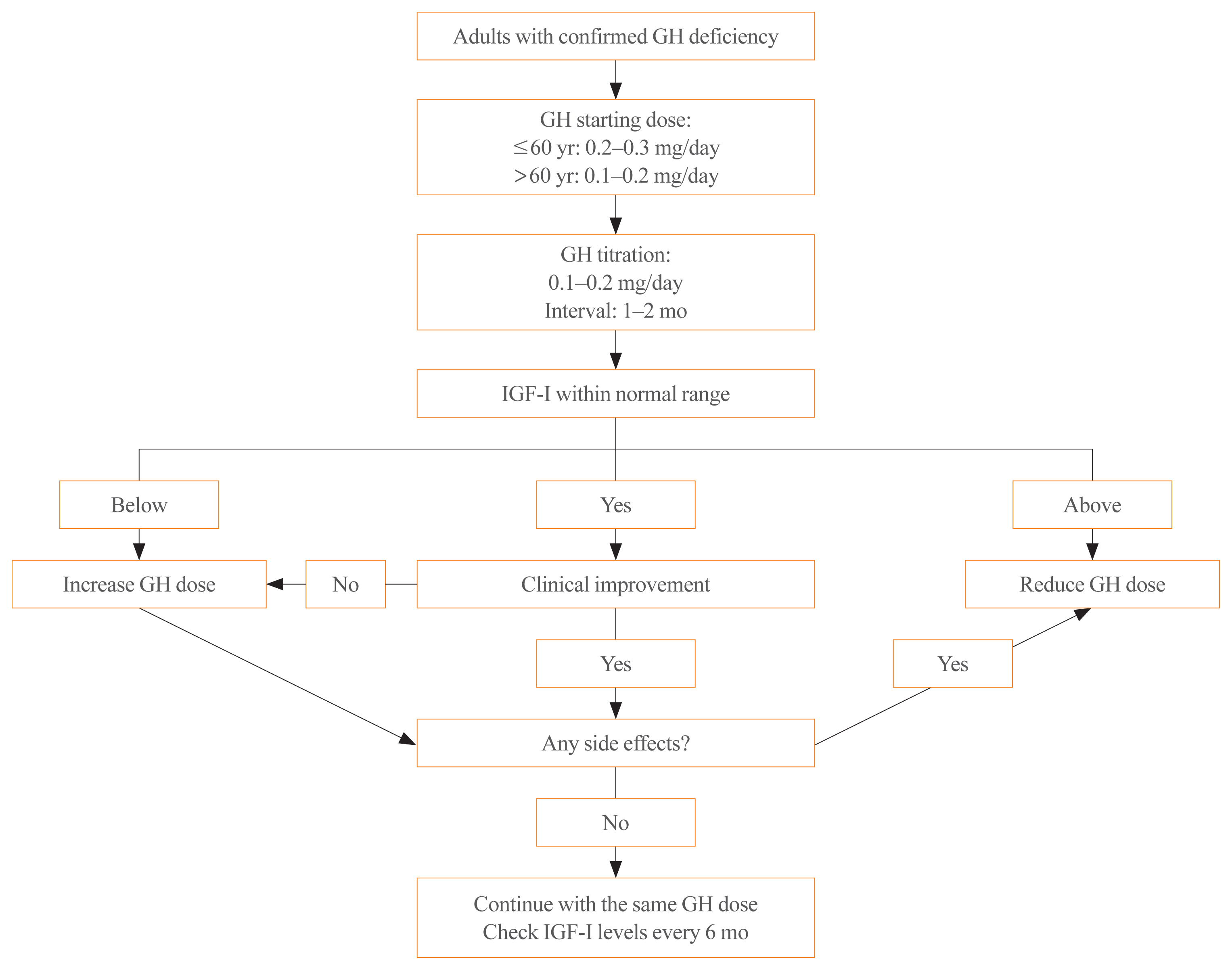
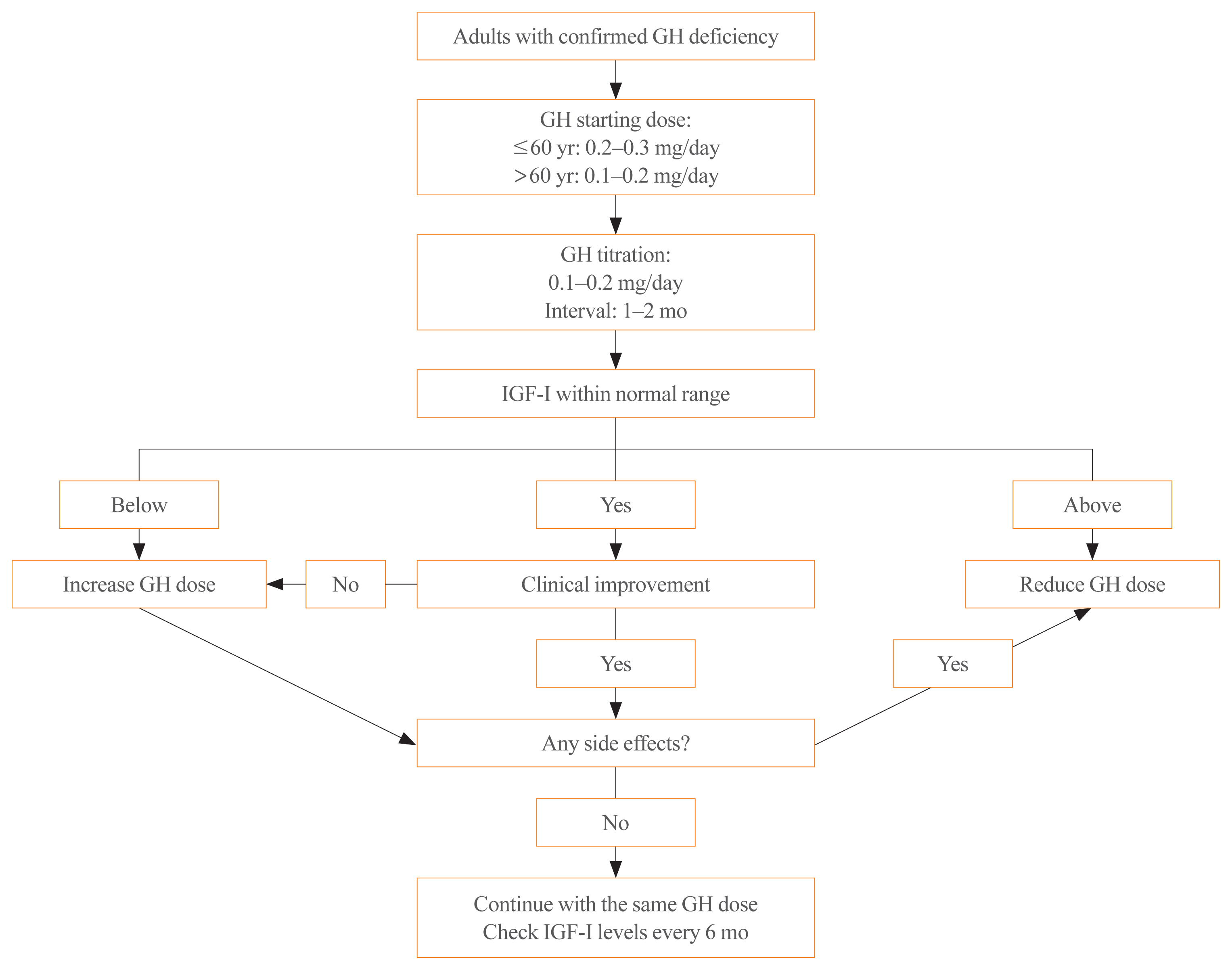
- Growth hormone (GH) deficiency is caused by congenital or acquired causes and occurs in childhood or adulthood. GH replacement therapy brings benefits to body composition, exercise capacity, skeletal health, cardiovascular outcomes, and quality of life. Before initiating GH replacement, GH deficiency should be confirmed through proper stimulation tests, and in cases with proven genetic causes or structural lesions, repeated GH stimulation testing is not necessary. The dosing regimen of GH replacement therapy should be individualized, with the goal of minimizing side effects and maximizing clinical improvements. The Korean Endocrine Society and the Korean Society of Pediatric Endocrinology have developed a position statement on the diagnosis and treatment of GH deficiency. This position statement is based on a systematic review of evidence and expert opinions.
-
Citations
Citations to this article as recorded by  - Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial
Ghina Tsurayya, Cut Alifiya Nazhifah, Muhammad Rahmat Pirwanja, Putri Oktaviani Zulfa, Muhammad Raihan Ramadhan Tatroman, Fajar Fakri, Muhammad Iqhrammullah
Children.2024; 11(2): 227. CrossRef - Evaluation of Adult Height in Patients with Non-Permanent Idiopathic GH Deficiency
Agnese Murianni, Anna Lussu, Chiara Guzzetti, Anastasia Ibba, Letizia Casula, Mariacarolina Salerno, Marco Cappa, Sandro Loche
Endocrines.2023; 4(1): 169. CrossRef - The effect of hypothalamic involvement and growth hormone treatment on cardiovascular risk factors during the transition period in patients with childhood-onset craniopharyngioma
Sang Hee Park, Yun Jeong Lee, Jung-Eun Cheon, Choong Ho Shin, Hae Woon Jung, Young Ah Lee
Annals of Pediatric Endocrinology & Metabolism.2023; 28(2): 107. CrossRef - Continuous Glucose Monitoring: A Possible Aid for Detecting Hypoglycemic Events during Insulin Tolerance Tests
Soo Yeun Sim, Moon Bae Ahn
Sensors.2023; 23(15): 6892. CrossRef - The risk patients with AGHD have of developing CVD
Eisha Javed, Maha Zehra, Naz Elahi
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 19: 200221. CrossRef - Diagnosis of GH Deficiency Without GH Stimulation Tests
Anastasia Ibba, Sandro Loche
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
Endocrinology and Metabolism.2022; 37(2): 359. CrossRef - A Radiomics-Based Model with the Potential to Differentiate Growth Hormone Deficiency and Idiopathic Short Stature on Sella MRI
Taeyoun Lee, Kyungchul Song, Beomseok Sohn, Jihwan Eom, Sung Soo Ahn, Ho-Seong Kim, Seung-Koo Lee
Yonsei Medical Journal.2022; 63(9): 856. CrossRef - Phenotypic spectrum of patients with mutations in CHD7: clinical implications of endocrinological findings
Ja Hye Kim, Yunha Choi, Soojin Hwang, Gu-Hwan Kim, Han-Wook Yoo, Jin-Ho Choi
Endocrine Connections.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2022; 37(6): 839. CrossRef - Laron syndrome: clinic, diagnostics (а clinical case)
P.M. Lіashuk, R.P. Lіashuk, N.I. Stankova, M.B. Kudina
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 193. CrossRef - Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan
Endocrinology and Metabolism.2021; 36(2): 322. CrossRef - Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
Endocrinology and Metabolism.2021; 36(3): 553. CrossRef - Asian Conference on Tumor Ablation guidelines for renal cell carcinoma
Byung Kwan Park, Shu-Huei Shen, Masashi Fujimori, Yi Wang
Investigative and Clinical Urology.2021; 62(4): 378. CrossRef - Diagnosis and Treatment of Adult Growth Hormone Deficiency
Jung Hee Kim
The Korean Journal of Medicine.2021; 96(5): 400. CrossRef
- Hypothalamus and Pituitary gland
- Medical Treatment with Somatostatin Analogues in Acromegaly: Position Statement
-
Sang Ouk Chin, Cheol Ryong Ku, Byung Joon Kim, Sung-Woon Kim, Kyeong Hye Park, Kee Ho Song, Seungjoon Oh, Hyun Koo Yoon, Eun Jig Lee, Jung Min Lee, Jung Soo Lim, Jung Hee Kim, Kwang Joon Kim, Heung Yong Jin, Dae Jung Kim, Kyung Ae Lee, Seong-Su Moon, Dong Jun Lim, Dong Yeob Shin, Se Hwa Kim, Min Jeong Kwon, Ha Young Kim, Jin Hwa Kim, Dong Sun Kim, Chong Hwa Kim
-
Endocrinol Metab. 2019;34(1):53-62. Published online March 21, 2019
-
DOI: https://doi.org/10.3803/EnM.2019.34.1.53
-
-
6,452
View
-
253
Download
-
8
Web of Science
-
11
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
The Korean Endocrine Society (KES) published clinical practice guidelines for the treatment of acromegaly in 2011. Since then, the number of acromegaly cases, publications on studies addressing medical treatment of acromegaly, and demands for improvements in insurance coverage have been dramatically increasing. In 2017, the KES Committee of Health Insurance decided to publish a position statement regarding the use of somatostatin analogues in acromegaly. Accordingly, consensus opinions for the position statement were collected after intensive review of the relevant literature and discussions among experts affiliated with the KES, and the Korean Neuroendocrine Study Group. This position statement includes the characteristics, indications, dose, interval (including extended dose interval in case of lanreotide autogel), switching and preoperative use of somatostatin analogues in medical treatment of acromegaly. The recommended approach is based on the expert opinions in case of insufficient clinical evidence, and where discrepancies among the expert opinions were found, the experts voted to determine the recommended approach. -
Citations
Citations to this article as recorded by  - Hydrogel-fiber-mesh-based 3D cell cultures: A new method for studying pituitary tumors
Wooju Jeong, Sungrok Wang, Yumin Kim, Soohyun Lee, Minhu Huang, Jaeil Park, Myung-Han Yoon, Chang-Myung Oh, Cheol Ryong Ku
Smart Materials in Medicine.2024;[Epub] CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
A Ram Hong, Ho-Cheol Kang
Endocrinology and Metabolism.2023; 38(2): 175. CrossRef - Growth Hormone Excess: Implications and Management
Suneela Dhaneshwar, Shrishti Shandily, Vatsalya Tiwari
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(6): 748. CrossRef - Revisiting the usefulness of the short acute octreotide test to predict treatment outcomes in acromegaly
Montserrat Marques-Pamies, Joan Gil, Elena Valassi, Marta Hernández, Betina Biagetti, Olga Giménez-Palop, Silvia Martínez, Cristina Carrato, Laura Pons, Rocío Villar-Taibo, Marta Araujo-Castro, Concepción Blanco, Inmaculada Simón, Andreu Simó-Servat, Gemm
Frontiers in Endocrinology.2023;[Epub] CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Octreotide in the treatment of acromegaly – the possibilities of high-dose therapy
I. A. Ilovayskaya
Meditsinskiy sovet = Medical Council.2022; (10): 148. CrossRef - Approach of Acromegaly during Pregnancy
Alexandru Dan Popescu, Mara Carsote, Ana Valea, Andreea Gabriela Nicola, Ionela Teodora Dascălu, Tiberiu Tircă, Jaqueline Abdul-Razzak, Mihaela Jana Țuculină
Diagnostics.2022; 12(11): 2669. CrossRef - Left to themselves: Time to target chronic pain in childhood rare diseases
Christine B. Sieberg, Alyssa Lebel, Erin Silliman, Scott Holmes, David Borsook, Igor Elman
Neuroscience & Biobehavioral Reviews.2021; 126: 276. CrossRef - Severe respiratory failure in a patient with COVID-19 and acromegaly: rapid improvement after adding octreotide
Jacob Luty, LesleAnn Hayward, Melanie Jackson, P Barton Duell
BMJ Case Reports.2021; 14(8): e243900. CrossRef - Precision Therapy in Acromegaly Caused by Pituitary Tumors: How Close Is It to Reality?
Cheol Ryong Ku, Vladimir Melnikov, Zhaoyun Zhang, Eun Jig Lee
Endocrinology and Metabolism.2020; 35(2): 206. CrossRef - Medical Treatment with Somatostatin Analogues in Acromegaly: Position Statement
Sang Ouk Chin, Cheol Ryong Ku, Byung Joon Kim, Sung-Woon Kim, Kyeong Hye Park, Kee Ho Song, Seungjoon Oh, Hyun Koo Yoon, Eun Jig Lee, Jung Min Lee, Jung Soo Lim, Jung Hee Kim, Kwang Joon Kim, Heung Yong Jin, Dae Jung Kim, Kyung Ae Lee, Seong-Su Moon, Dong
The Korean Journal of Medicine.2019; 94(6): 485. CrossRef
- A Case of Simultaneous Presentation of Thyroid Crisis and Diabetic Ketoacidosis.
-
Kyung Ae Lee, Kyung Taek Park, Hea Min Yu, Heung Yong Jin, Ji Hyun Park, Hong Sun Baek, Tae Sun Park
-
Endocrinol Metab. 2012;27(1):63-67. Published online March 1, 2012
-
DOI: https://doi.org/10.3803/EnM.2012.27.1.63
-
-
2,085
View
-
31
Download
-
1
Crossref
-
 Abstract Abstract
 PDF PDF
- Two important endocrine emergencies, thyroid crisis and diabetic ketoacidosis (DKA), are uncommon when presented together, but pose serious complications. Without appropriate management, they may result in high mortality. Although several cases of simultaneous presentation of thyroid crisis and DKA have been reported, it is a clinically unusual situation and remains a diagnostic and management challenge in clinical practice. We report rare case with simultaneous presentation of thyroid crisis and DKA without previous warning symptoms. A 23-year-old-woman was brought to the emergency department presenting with acute abdominal pain for one day. She was healthy and there was no personal history of diabetes or thyroid disease. Through careful physical examination and laboratory tests, the patient was diagnosed with thyroid crisis combined with DKA. Concomitance of these two endocrine emergencies led to sudden cardiac arrest, but she was successfully resuscitated. This emphasizes the importance of early recognition and prompt management when the two diseases are presented concomitantly.
-
Citations
Citations to this article as recorded by  - Health Behaviors and Risk Factors Associated with Chronic Kidney Disease in Korean Patients with Diabetes: The Fourth Korean National Health and Nutritional Examination Survey
Suk Jeong Lee, Chae Weon Chung
Asian Nursing Research.2014; 8(1): 8. CrossRef
|